nutrition
In 2022, I graduated from nursing school with dreams of starting my career as a nurse. However, life had other plans. I was diagnosed with gastroparesis, a condition that made it impossible for me to work and pursue my passion. As my condition worsened, I had to put my career on hold to focus on my health.
 Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
My local registered dietitian recommended Parenteral Nutrition (PN) and sent the order. We were then referred to Option Care Health (OPCH). I was scared to start PN, but my OPCH dietitian reassured me, saying, “Just because you’re on PN doesn’t mean your life is over. The goal is to give you back more of your life than before.” Her words stuck with me, offering hope during a difficult time.
Due to my blood sugar issues, I’m on 23-hour PN feeds and carry a backpack that has become a part of me. Despite these challenges, my OPCH team has been incredible. My registered dietitian and pharmacist have truly been lifesavers. I continue to speak with my OPCH registered dietitian weekly because she genuinely cares about my well-being and supports me through every step of my journey.
Thanks to the unwavering support of my Option Care Health team and my local registered dietitian, I am back to work and feeling so much better. I wholeheartedly recommend Option Care Health to anyone in need. They have played a crucial role in my recovery, and I am forever grateful for their dedication and care.

nutrition
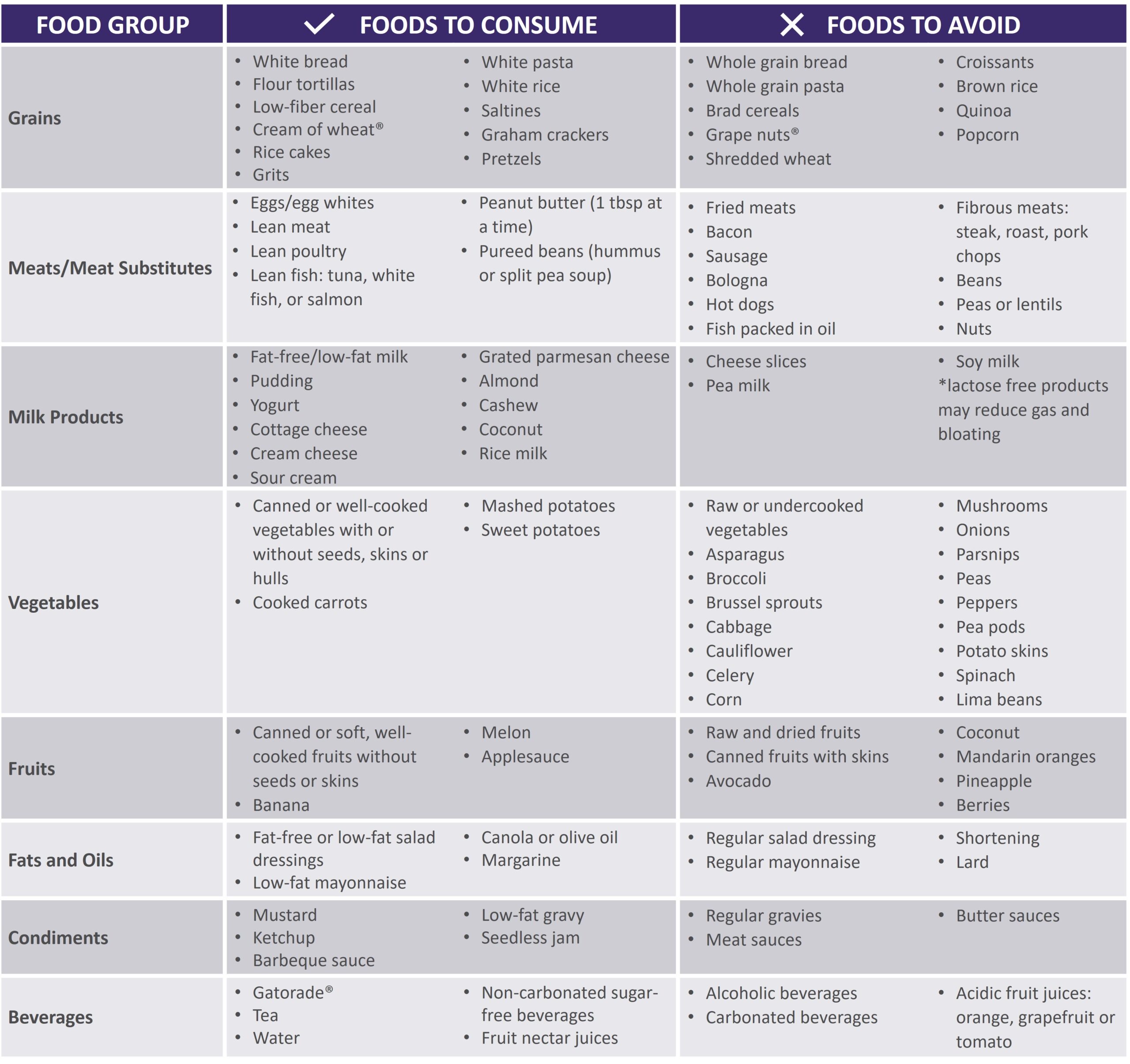
Gastroparesis refers to a delay in emptying stomach contents. Symptoms often include feeling full after eating a meal, or even a small amount of food, as well as nausea, vomiting, bloating or abdominal pain. The causes of gastroparesis may include diabetes mellitus, complications after surgery, kidney disease, certain medications, thyroid disorders, cancer, among others.
The following tips are intended to reduce symptoms and help maintain adequate nutrition.
|
Mealtime
|
||
|
Foods
|
|
|
Fluids
- Stay hydrated. Most adults need 6-10 cups of water per day. Sip slowly throughout the day.
- Drink fluids with meals, however; be sure not to fill up on liquids
- Avoid carbonated beverages as they can cause bloating
Otro
- Avoid alcohol as it can affect stomach emptying
- Foods that are acidic, spicy, or contain caffeine or mint may increase acid reflux
- Keep blood sugars under control if you have diabetes
- Keep a food diary to track your intake and find foods that are best tolerated
- Exercise may increase stomach emptying and reduce symptoms. Walking after meals is suggested.
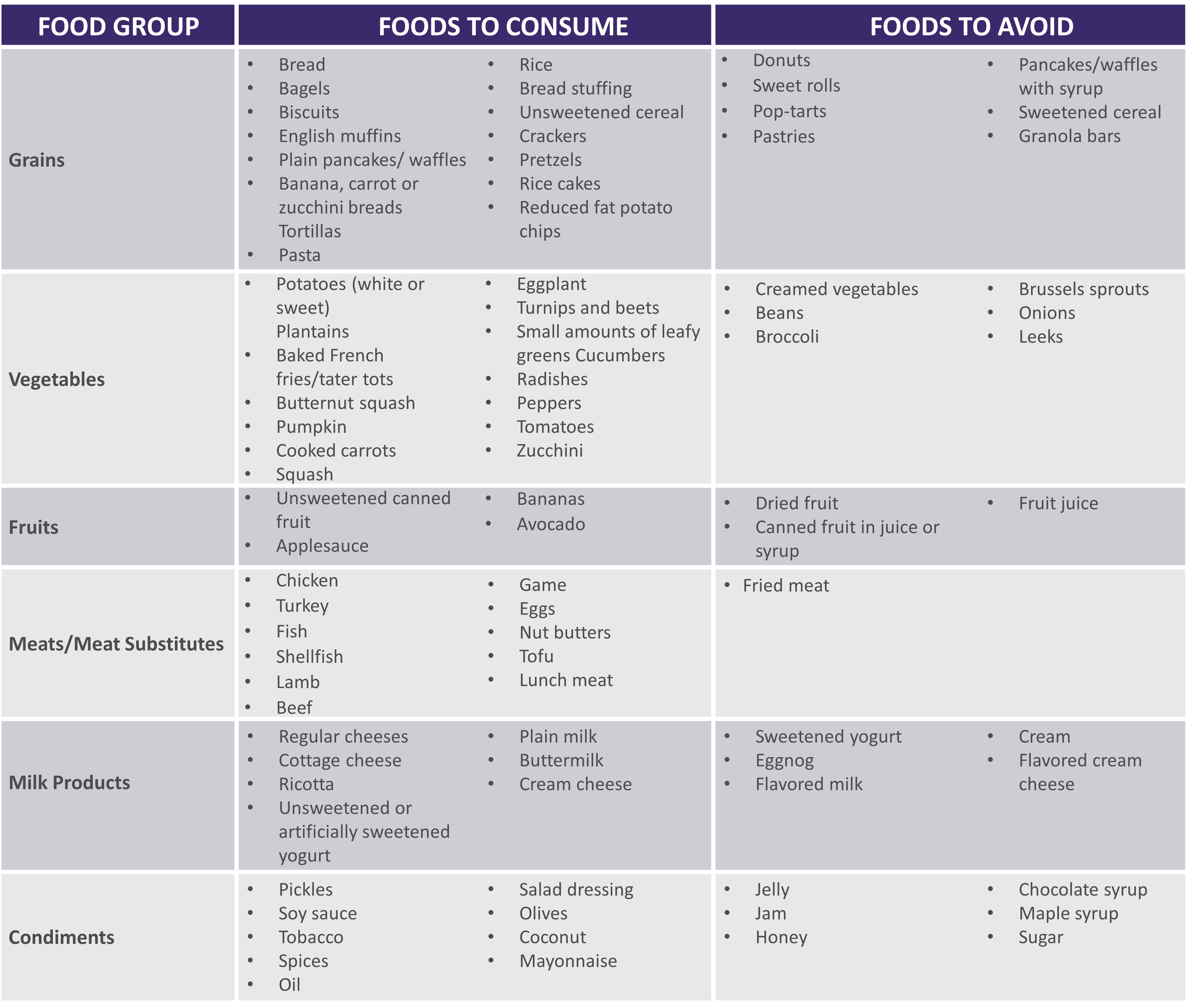
See below for help in choosing more optimal foods from each food group:
 |
|
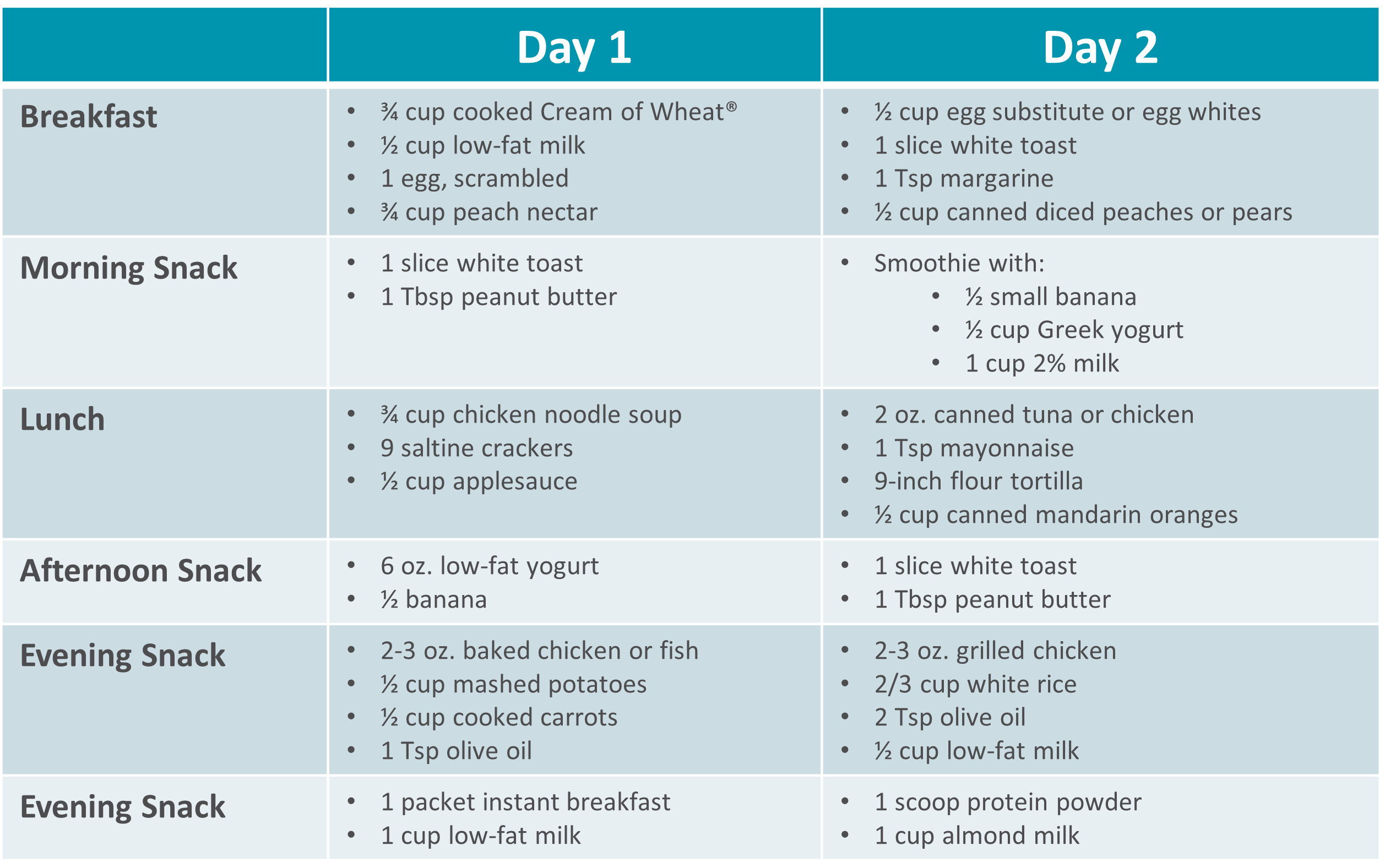
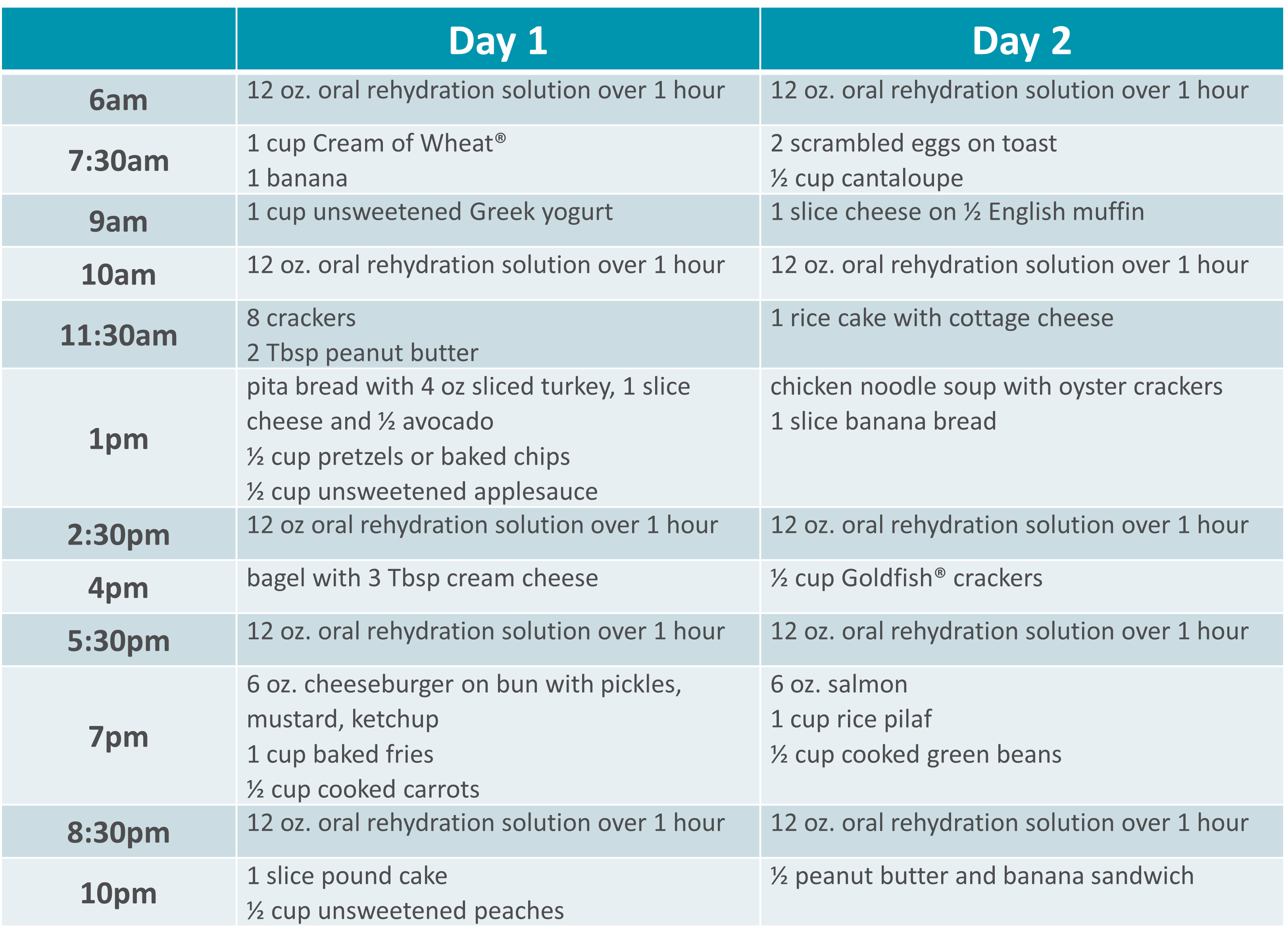
Gastroparesis Sample Menus |
 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

nutrition
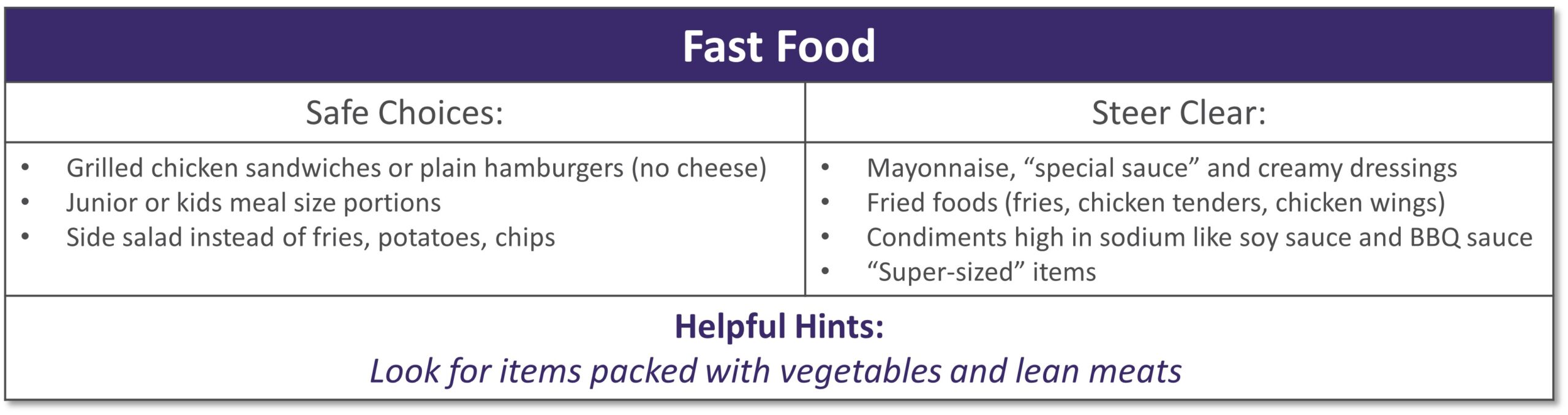
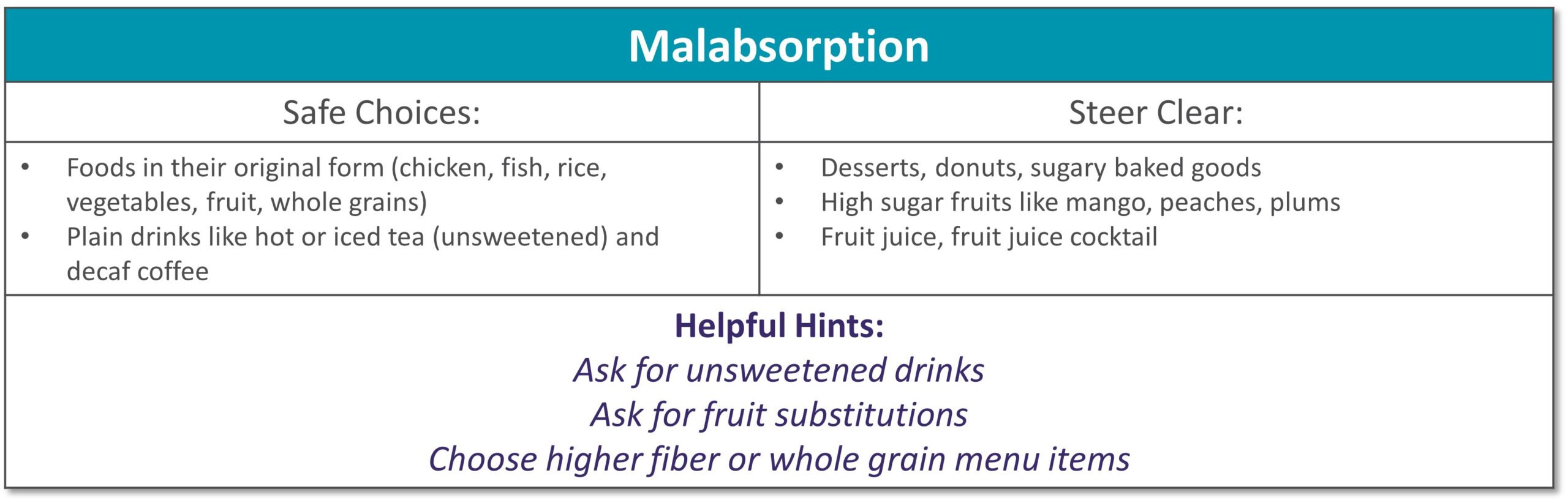
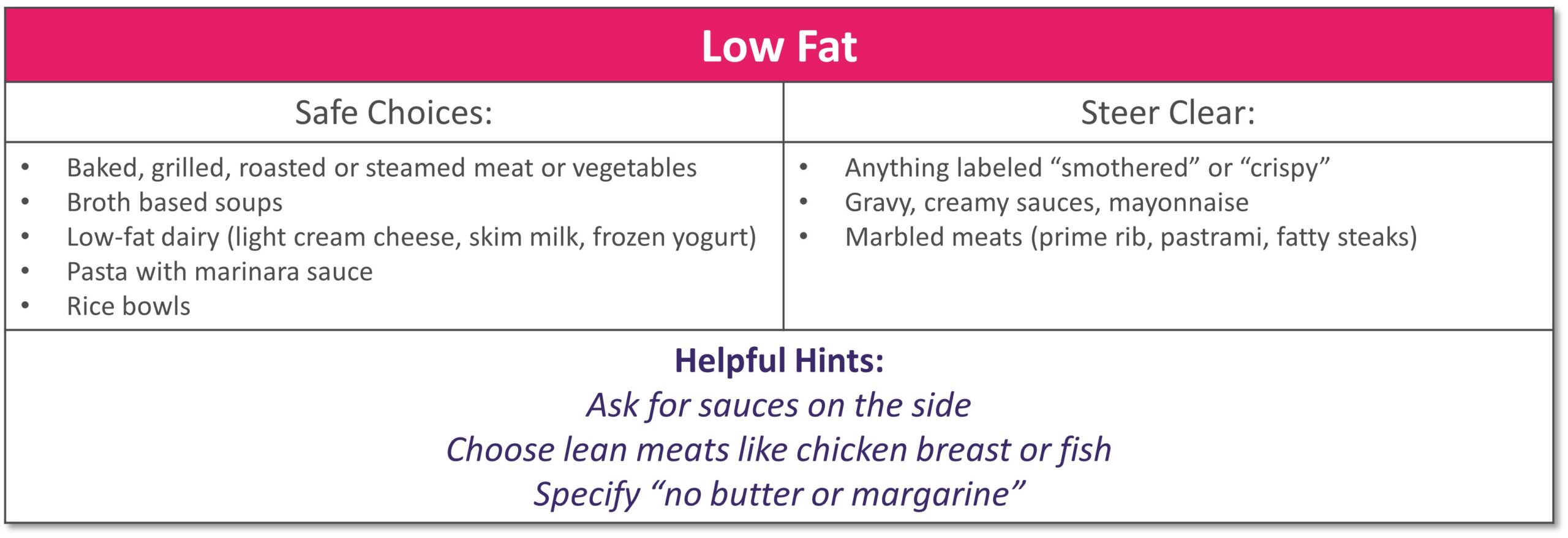
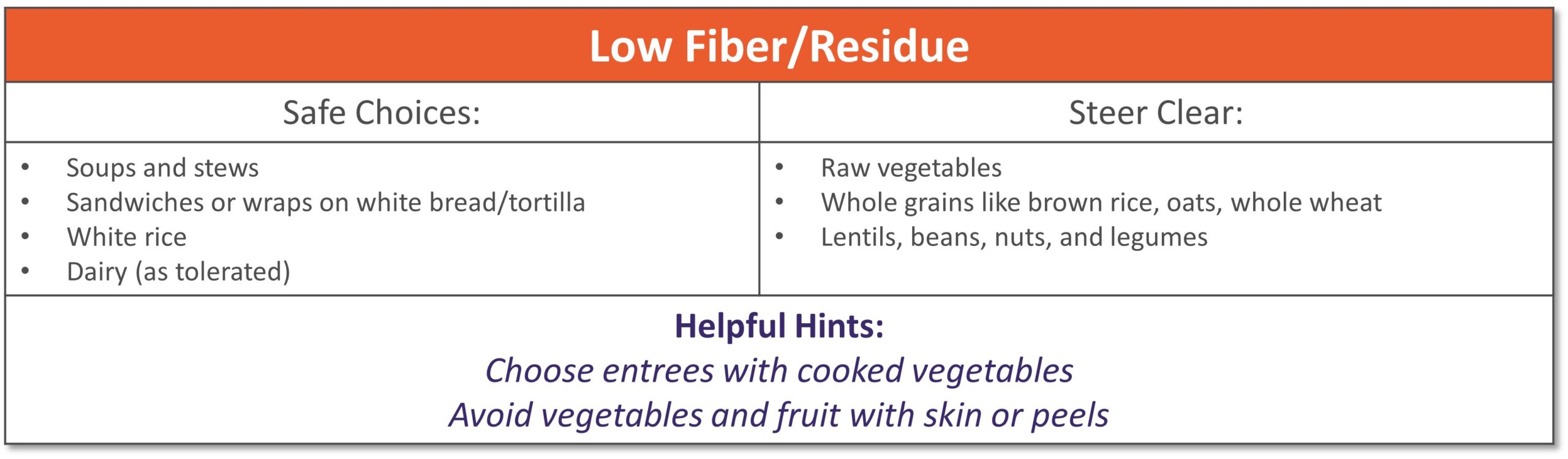
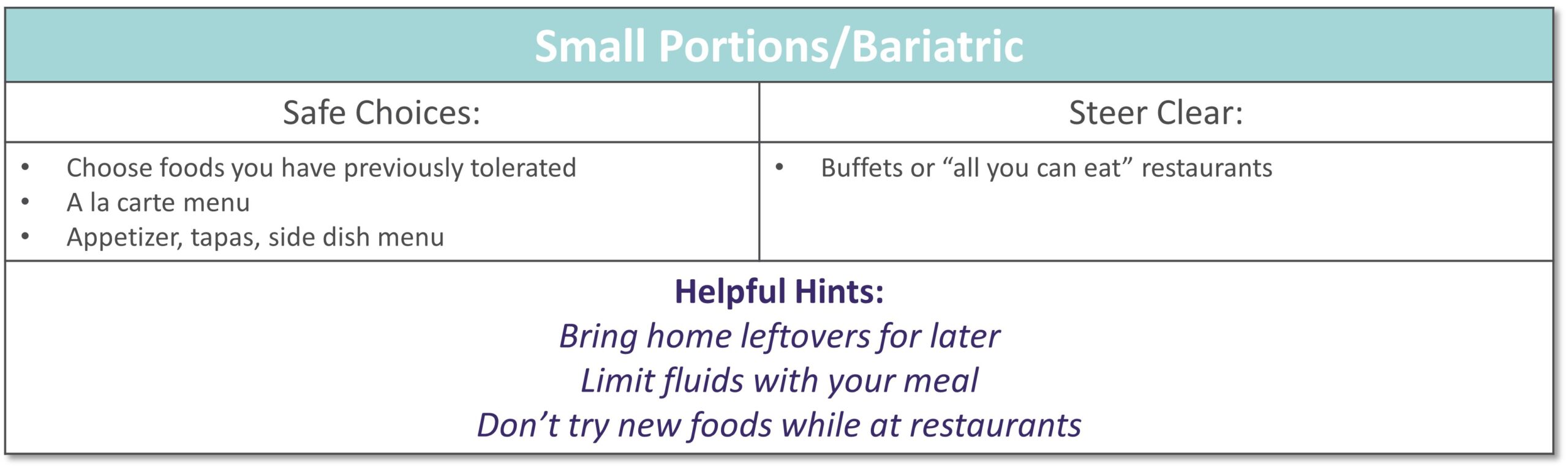
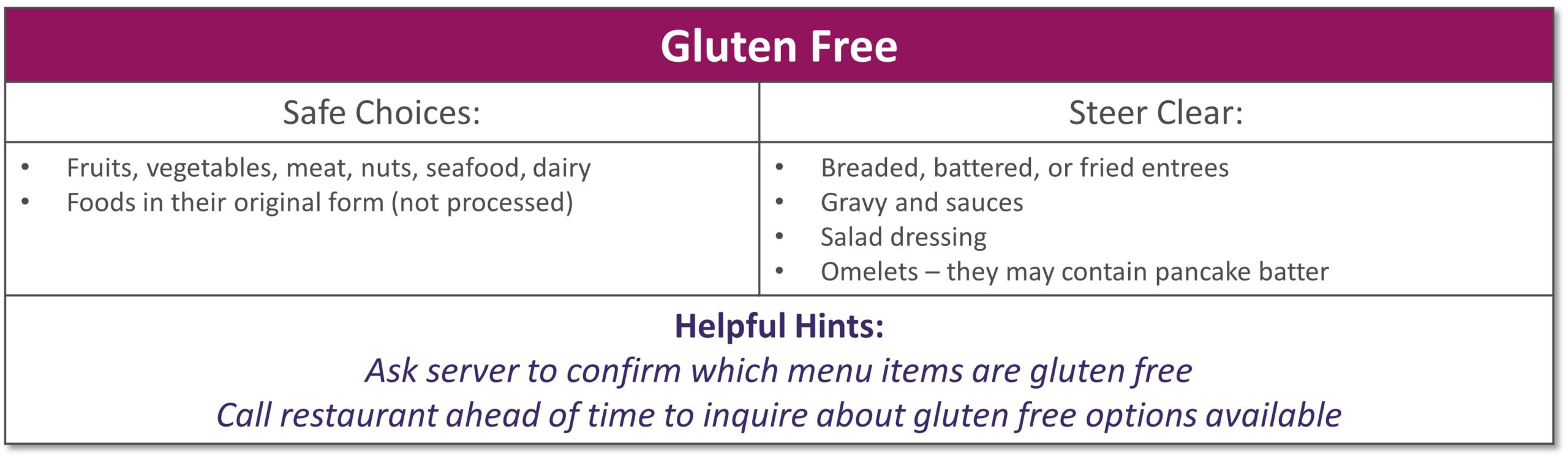
Dining out at restaurants is a nice treat but also challenging when trying to stick with your therapeutic diet, especially with gastrointestinal diseases. Most restaurants have menus and nutritional information available online. Restaurants are not required to have nutrition information available if they have less than 20 locations. Follow these tips to navigate eating out if you have specialized nutrition needs.
GENERAL TIPS:
- Research the menu online
- Pick a cuisine you tolerate
- Ask server for nutritional information or ingredients if not listed on the menu
- Do NOT be afraid to ask to customize the meal or ask for specific changes
- Communicate with wait staff if you have a food allergy or intolerance
- HAVE A PLAN AND STICK WITH IT!
|
|
|
|
|
|
|
|
|
|
|
|
|
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health. *This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information. |

nutrition
Short bowel syndrome (SBS), or intestinal failure, is a condition in which your body is unable to absorb enough nutrients from foods and fluids you consume. This can occur after a surgical resection or damage to your intestines. Symptoms and absorption vary by individual based on the amount and health of the remaining intestine. Symptoms of SBS can include diarrhea, dehydration, electrolyte abnormalities, and weight loss.
The following tips are intended to maximize absorption, improve your nutritional status and reduce dependence on parenteral nutrition.
- Mealtime
- Eat small, frequent meals (6-8 per day)
- Foods
- Eat protein at all meals: eggs, creamy peanut butter, chicken, fish, beef, tofu
- Choose complex carbohydrates such as bread, pasta, rice, and potatoes
- Limit raw vegetables to small amounts
- Avoid fruits with skin or edible seeds
- Limit raw fruits to very small portion twice a day
- Increase your soluble fiber to thicken output with foods such as bananas, applesauce, rice, oatmeal or use of soluble fiber supplements
- Avoid high fat foods such as fried foods if your colon is intact
- Use caution with dairy products – lactose intolerance is common with SBS
- Avoid concentrated sweets such as candy, desserts, and juice
- Avoid foods artificially sweetened with sorbitol or mannitol (Splenda® is okay)
- Fluids
- Drink isotonic fluids (with electrolytes), ideally oral rehydration solutions (see recipes below)
- Do not drink fluids with meals as it increases how quickly food passes through
- Limit to 4 oz. fluid during your meal to allow your food to be best absorbed
- Drink ½ hour before or 2 hours after eating
- If you do not have your colon, your fluid losses will be higher
- Otro
- If prescribed by your doctor, take antidiarrheal medication ½ hour before meals
- Salty foods such as pretzels or soups are usually well tolerated and help absorb fluid
- Avoid caffeine and alcohol
See below for help in choosing more optimal foods from each food group:
 |
|
|
|
**For homemade ORS, discard after 24 hours if not consumed **Visit for more recipes: https://optioncarehealth.com/patients/resources/sbs-friendly-recipes |
SBS Sample Menu |
 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.