Apoyo nutricional
Gastroparesis refers to a delay in emptying stomach contents. Symptoms often include feeling full after eating a meal, or even a small amount of food, as well as nausea, vomiting, bloating or abdominal pain. The causes of gastroparesis may include diabetes mellitus, complications after surgery, kidney disease, certain medications, thyroid disorders, cancer, among others.
The following tips are intended to reduce symptoms and help maintain adequate nutrition.
|
Mealtime
|
||
|
Foods
|
|
|
Fluids
- Stay hydrated. Most adults need 6-10 cups of water per day. Sip slowly throughout the day.
- Drink fluids with meals, however; be sure not to fill up on liquids
- Avoid carbonated beverages as they can cause bloating
Otro
- Avoid alcohol as it can affect stomach emptying
- Foods that are acidic, spicy, or contain caffeine or mint may increase acid reflux
- Keep blood sugars under control if you have diabetes
- Keep a food diary to track your intake and find foods that are best tolerated
- Exercise may increase stomach emptying and reduce symptoms. Walking after meals is suggested.
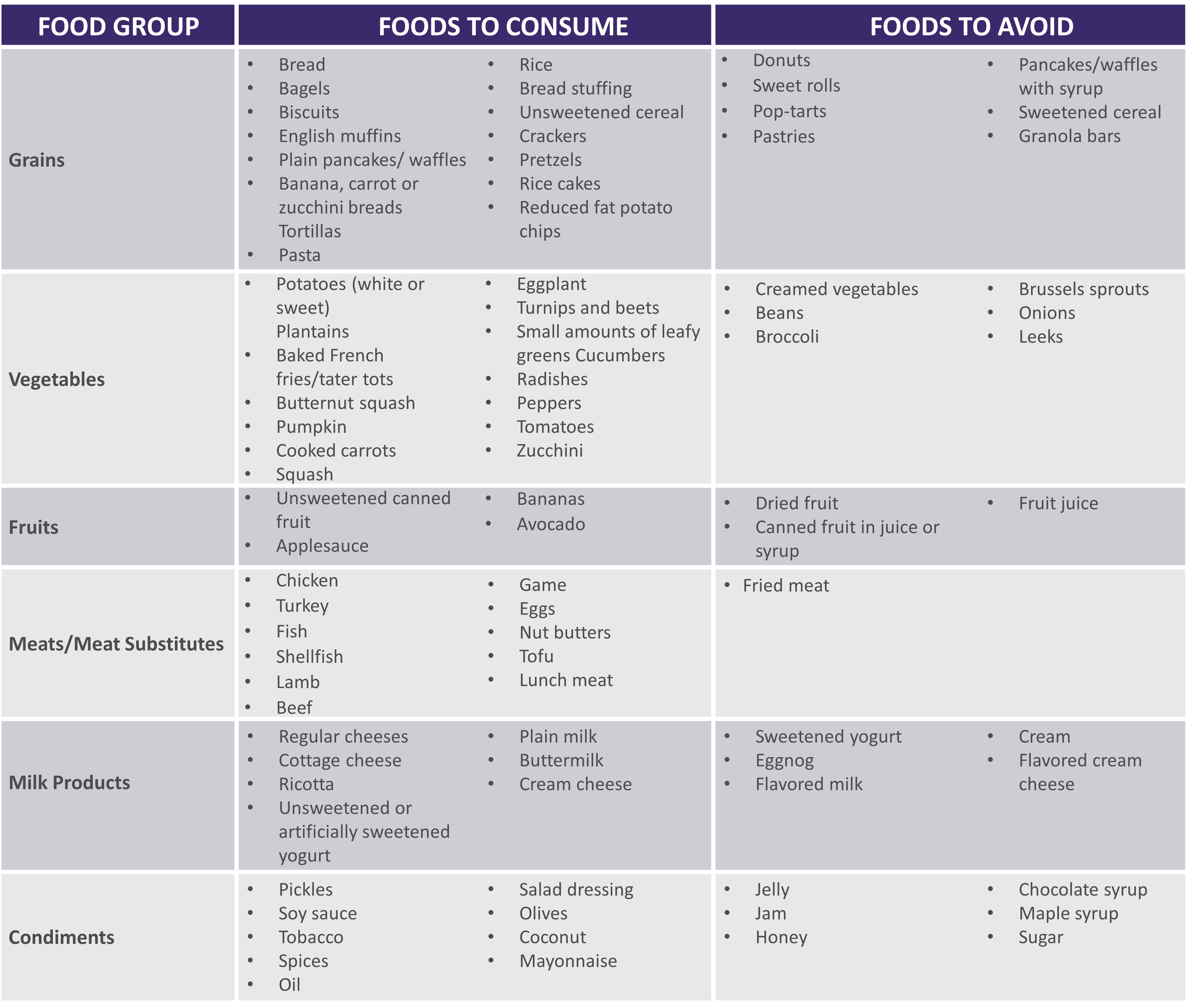
See below for help in choosing more optimal foods from each food group:
 |
|
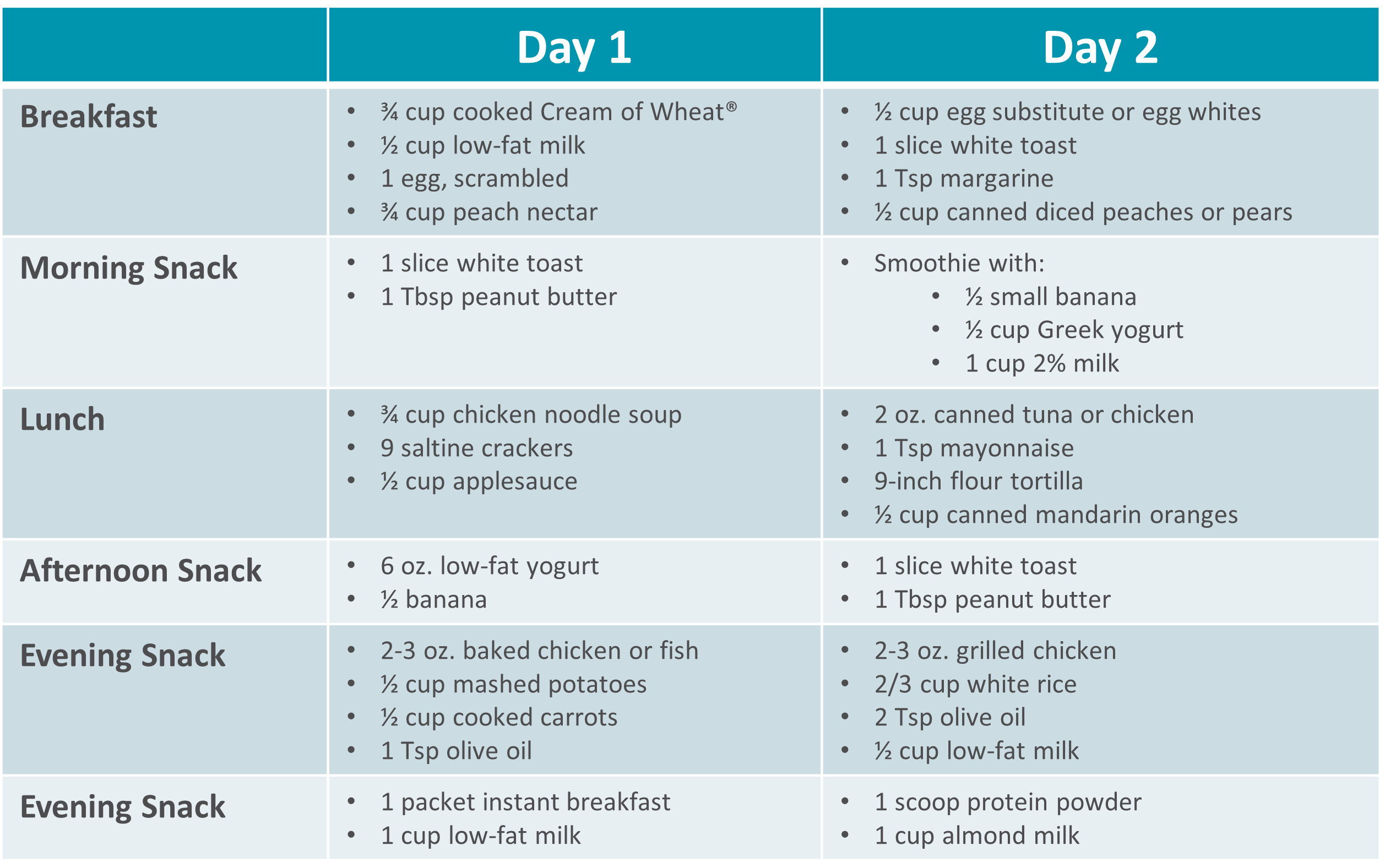
Gastroparesis Sample Menus |
 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

Apoyo nutricional
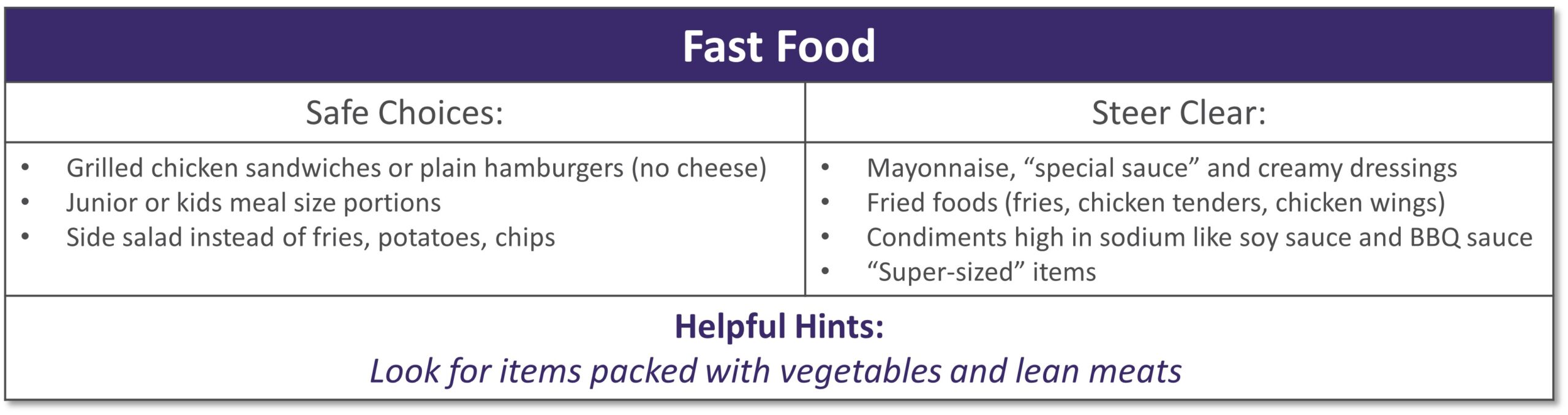
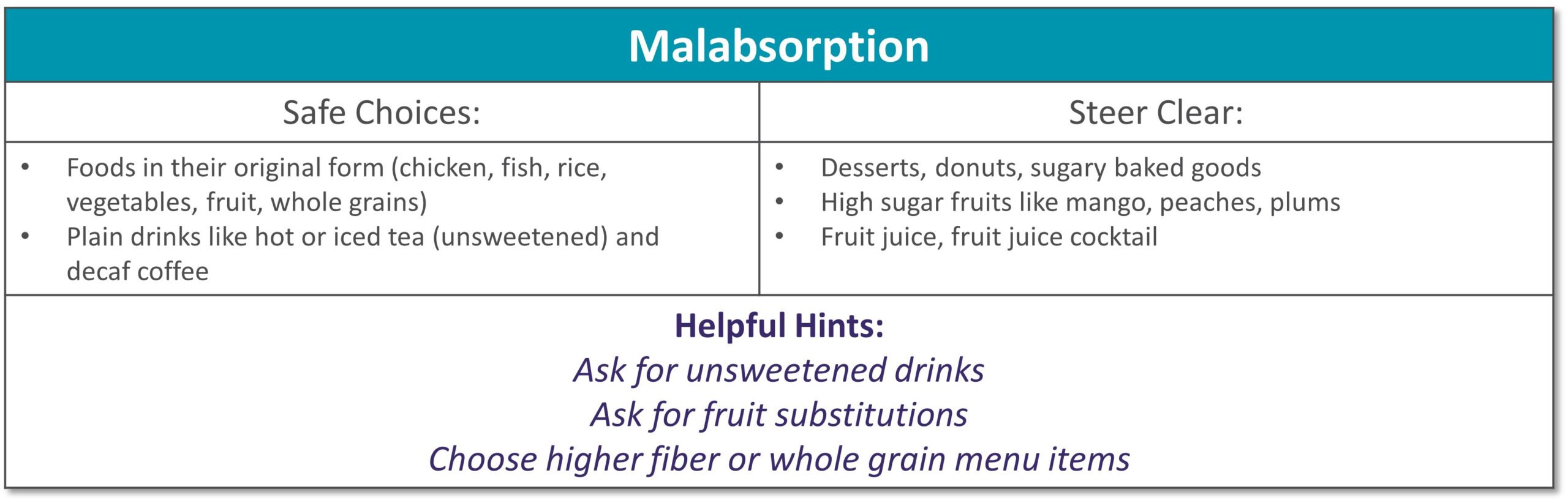
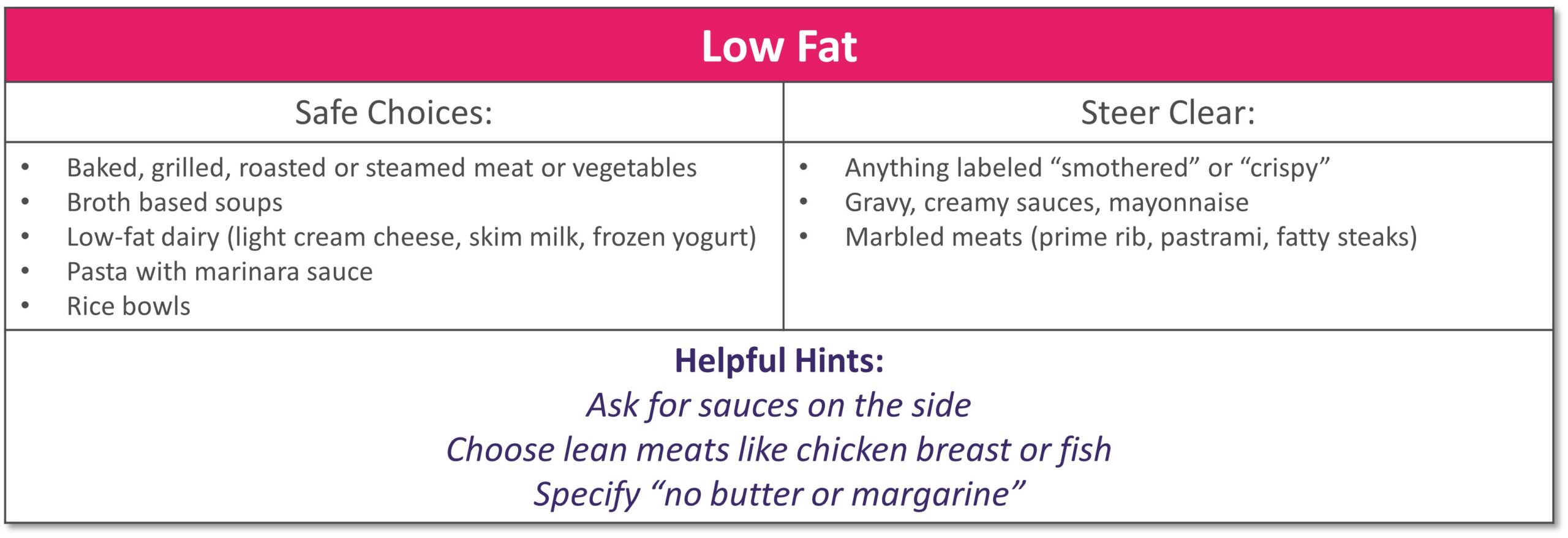
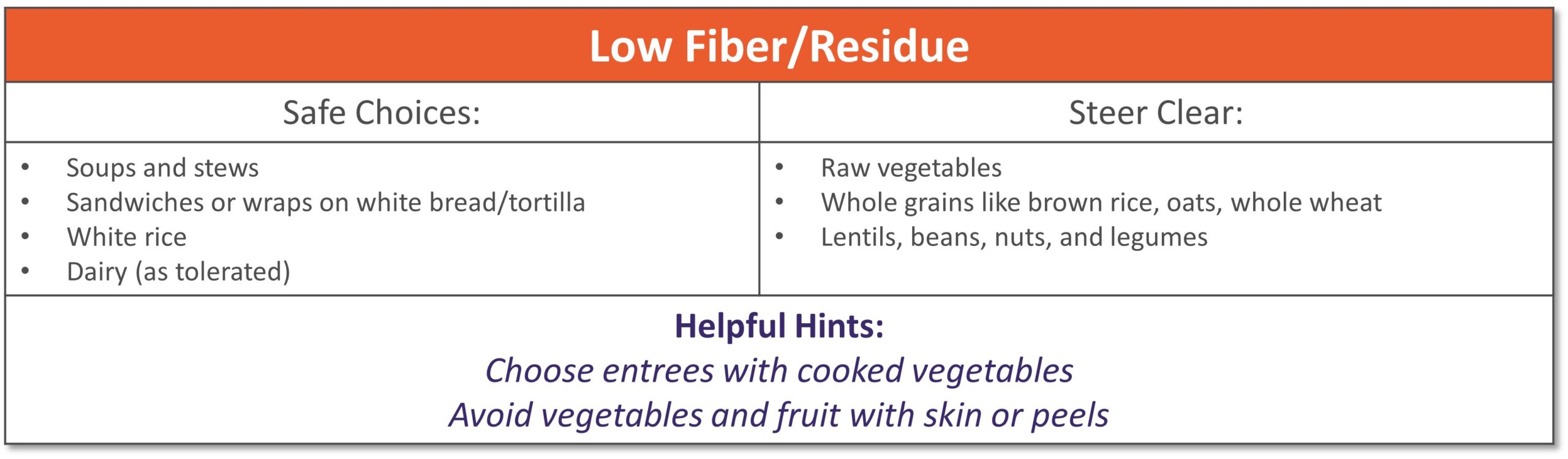
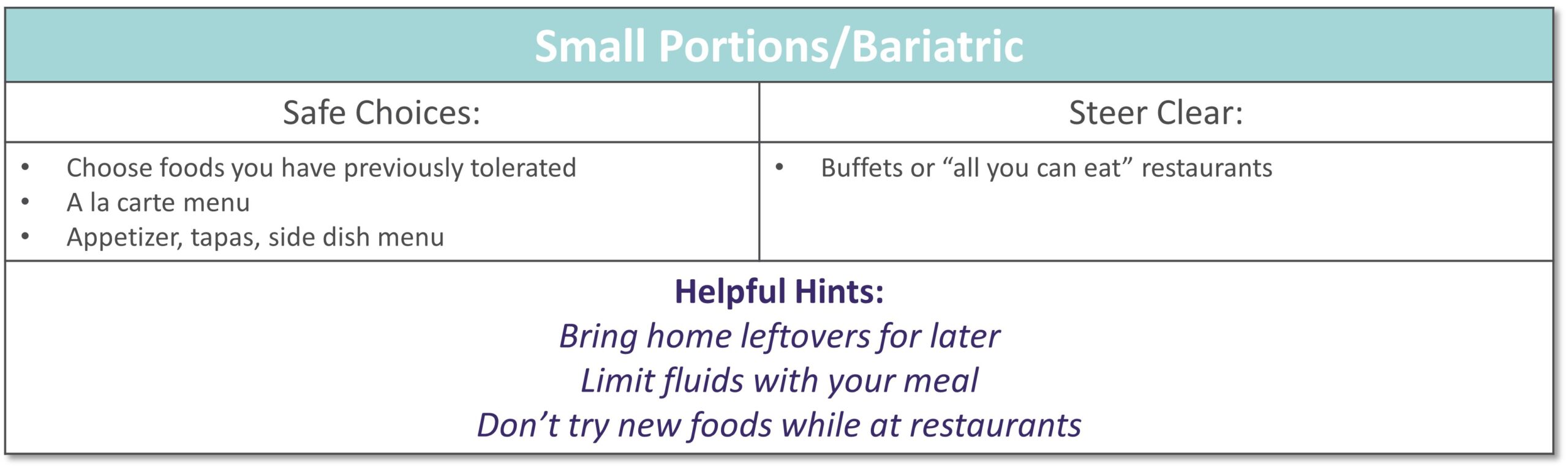
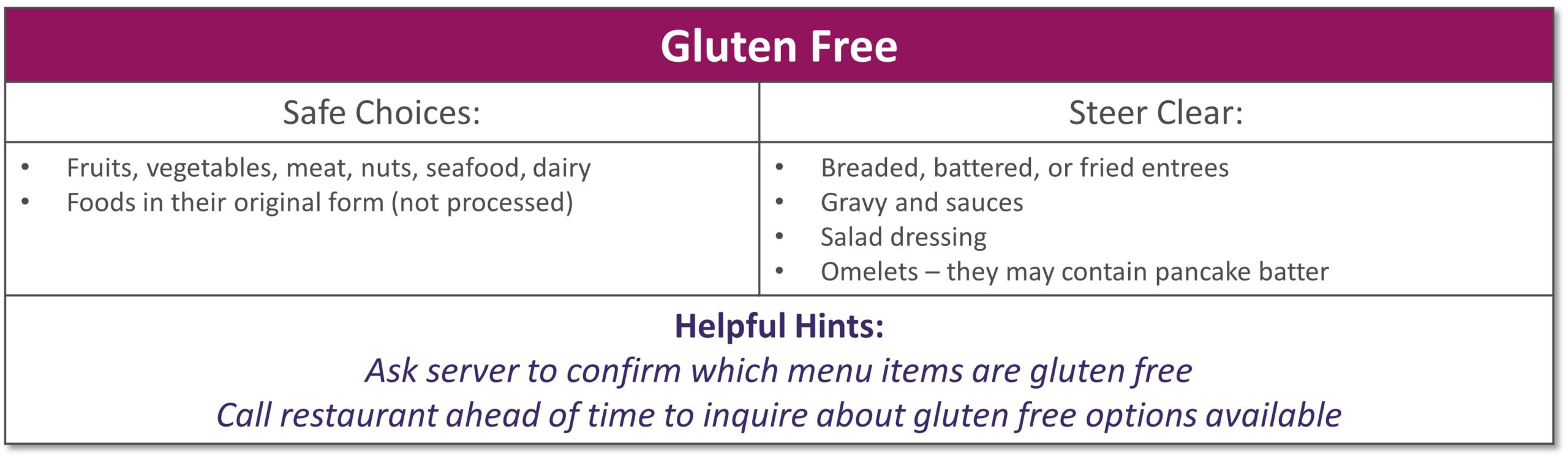
Dining out at restaurants is a nice treat but also challenging when trying to stick with your therapeutic diet, especially with gastrointestinal diseases. Most restaurants have menus and nutritional information available online. Restaurants are not required to have nutrition information available if they have less than 20 locations. Follow these tips to navigate eating out if you have specialized nutrition needs.
GENERAL TIPS:
- Research the menu online
- Pick a cuisine you tolerate
- Ask server for nutritional information or ingredients if not listed on the menu
- Do NOT be afraid to ask to customize the meal or ask for specific changes
- Communicate with wait staff if you have a food allergy or intolerance
- HAVE A PLAN AND STICK WITH IT!
|
|
|
|
|
|
|
|
|
|
|
|
|
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health. *This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information. |

Apoyo nutricional
Short bowel syndrome (SBS), or intestinal failure, is a condition in which your body is unable to absorb enough nutrients from foods and fluids you consume. This can occur after a surgical resection or damage to your intestines. Symptoms and absorption vary by individual based on the amount and health of the remaining intestine. Symptoms of SBS can include diarrhea, dehydration, electrolyte abnormalities, and weight loss.
The following tips are intended to maximize absorption, improve your nutritional status and reduce dependence on parenteral nutrition.
- Mealtime
- Eat small, frequent meals (6-8 per day)
- Foods
- Eat protein at all meals: eggs, creamy peanut butter, chicken, fish, beef, tofu
- Choose complex carbohydrates such as bread, pasta, rice, and potatoes
- Limit raw vegetables to small amounts
- Avoid fruits with skin or edible seeds
- Limit raw fruits to very small portion twice a day
- Increase your soluble fiber to thicken output with foods such as bananas, applesauce, rice, oatmeal or use of soluble fiber supplements
- Avoid high fat foods such as fried foods if your colon is intact
- Use caution with dairy products – lactose intolerance is common with SBS
- Avoid concentrated sweets such as candy, desserts, and juice
- Avoid foods artificially sweetened with sorbitol or mannitol (Splenda® is okay)
- Fluids
- Drink isotonic fluids (with electrolytes), ideally oral rehydration solutions (see recipes below)
- Do not drink fluids with meals as it increases how quickly food passes through
- Limit to 4 oz. fluid during your meal to allow your food to be best absorbed
- Drink ½ hour before or 2 hours after eating
- If you do not have your colon, your fluid losses will be higher
- Otro
- If prescribed by your doctor, take antidiarrheal medication ½ hour before meals
- Salty foods such as pretzels or soups are usually well tolerated and help absorb fluid
- Avoid caffeine and alcohol
See below for help in choosing more optimal foods from each food group:
 |
|
|
|
**For homemade ORS, discard after 24 hours if not consumed **Visit for more recipes: https://optioncarehealth.com/patients/resources/sbs-friendly-recipes |
SBS Sample Menu |
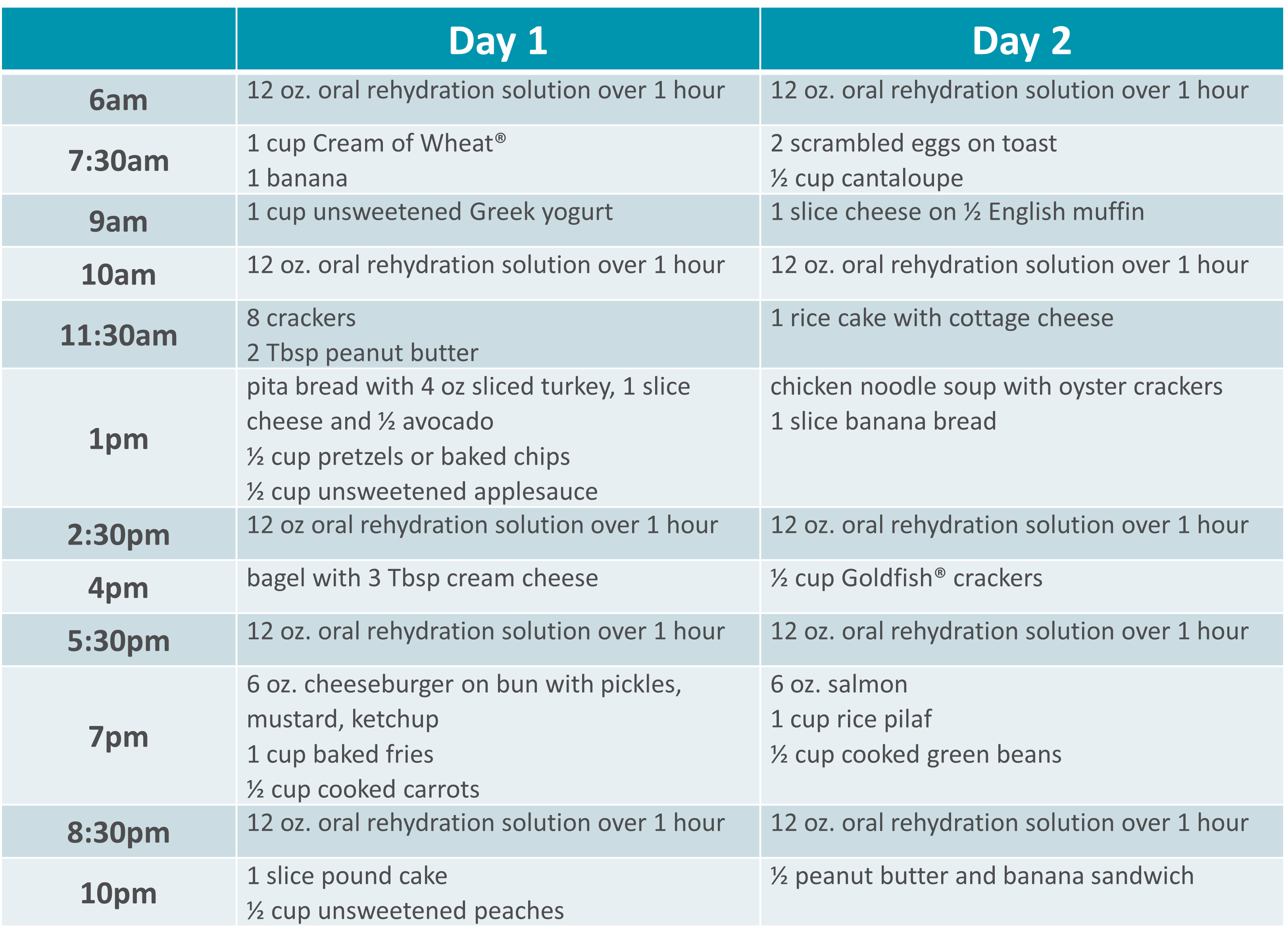 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

Apoyo nutricional
Gillian was just 11 years old when she began treatment for multiple complex chronic illnesses. As a teenager, she was diagnosed with gastrointestinal (GI) motility disorder and gastroparesis, which led to long-term, severe malnutrition.
“It was really hard missing out on so many activities growing up. I was prescribed various medications and tube feedings, but nothing helped long term. By early adulthood my symptoms worsened so I had to withdraw from college and take an extended medical leave from my job,” she said.
From 2015 to 2018, Gillian’s health progressively declined. “I was on tube feeds and other intravenous (IV) medications at the time. I began losing weight again, my neurological function was declining and I couldn’t speak or walk.” As Gillian’s health continued to decline, she found the strength to advocate for herself and build upon her excellent team of healthcare providers.
Gillian was put on total parenteral nutrition (TPN) in 2018, managed by Option Care Health. “This was my turning point. Today my labs are perfect and my cognitive function is back to normal. My weight has stabilized and I’m back to living life. I owe so much of my progress to my Option Care Health team.” Gillian continued, “My registered dietitian (RD) is amazing. During the initial COVID outbreak, I was struggling with my health and I couldn’t reach my doctors, but my Option Care Health RD was there every time I reached out. I got the help I needed and I owe it all to her.”
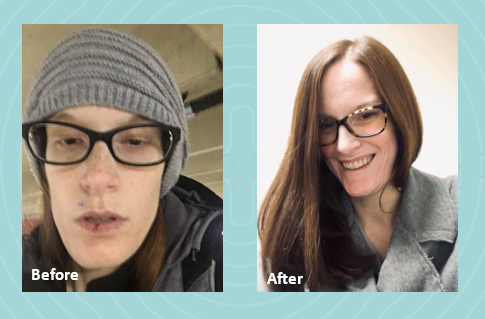
She claims that her Option Care Health team including her pharmacist and pharmacy technician go above and beyond expectation. “Other companies and even providers don’t always focus on how the patient needs to be living their best quality of life during treatment. My team at Option Care Health set up my deliveries in the evening to accommodate my work schedule. They also deliver them upstairs to me because I’m unable to carry them. My pharmacist and tech were so helpful this summer. They were able to find a way for me to go on vacation by switching around my infusions and supplies. Thanks to their help, I was able to go on my first trip since 2015! They are really focused on me as a person, not just a patient.”
Her message to her Option Care Health team is one of gratitude, “I just want them all to know how appreciative I am. They have and continue to be a key part of my recovery and I couldn’t be more grateful.” Gillian is thriving and living her best quality of life. She’s working, volunteering and spending as much time as possible with family and friends.
Learn more about malnutrition and join us in spreading awareness this ASPEN Malnutrition Awareness Week*, September 19th-23rd: ASPENMAW22
Semana de Concientización sobre la Desnutrición™ es una marca de la American Society for Parenteral & Enteral Nutrition (ASPEN). Se utiliza con permiso de la ASPEN.

Apoyo nutricional
 La nutrición clínica no es un esfuerzo solitario.
La nutrición clínica no es un esfuerzo solitario.
En Option Care Health, nuestros nutricionistas registrados son una parte fundamental del equipo de apoyo nutricional. Ellos trabajan con enfermeros, farmacéuticos y otros profesionales clínicos para ofrecer la mejor atención a nuestros pacientes, ya sea en el hospital o en su hogar.
Nos centramos en un enfoque de colaboración porque sabemos que es muy eficaz para los pacientes y apoya resultados óptimos.
Haga clic en el siguiente enlace para leer el artículo publicado en Today's Dietitian.

Apoyo nutricional
After overcoming ovarian cancer in 1995, retired nurse Lydia Zwilling found herself facing an arduous battle to reclaim her health. Nearly a quarter million women are diagnosed with ovarian cancer every year and for most, treatment goes according to plan. Unfortunately, some like Lydia, experience complications that last a lifetime.
While radiation therapy may have saved Lydia’s life, it also burned her small intestine and contributed to complications that ultimately caused her kidneys to fail. She had to be put on dialysis for two years before she was able to receive a kidney transplant in 2006.
Doctors also had to remove the burned portion of her small intestine, leaving her with just three functioning feet of her bowel. Diagnosed with short bowel syndrome (SBS), Lydia started to experience dramatic weight loss because her body could no longer absorb adequate nutrition. At 72 pounds, she was emaciated and unable to regain any weight. She became home-bound.
“I felt deeply frustrated,” Lydia said. “After beating a life-threatening cancer, I still had no strength or energy. I decided it was time to take some action to see what could make me better.”
In 2006, Lydia was introduced to Option Care by her attending physician and put on total parenteral nutrition (TPN), which gives her the nutrition she needs through intravenous delivery.
“TPN made an immediate difference in my overall health,” Lydia said. “I finally started to feel like myself again.”
Lydia and her husband are registered nurses so they are able to handle her TPN treatments and labs from home, self-infusing five days a week for nine hours at night. Lydia works closely with her care team at Option Care to receive additional antibiotics when she needs them. They also coordinate directly with her physicians to communicate any changes in her treatment.
“After many years with Option Care as my infusion provider, I’ve developed a close relationship with my care team and we’ve gotten to know each other on a personal level,” Lydia said. “You can tell that they care about what is going on with me and not just my medical health. I have complete confidence in their abilities to provide me with the best care possible.”
As a grateful cancer survivor, Lydia is thriving thanks to TPN. She credits her involvement with Option Care as enabling her to regain a near normal life. She is now able to visit her grandchildren who live six and a half hours away as well as escape the cold Minnesota winters for vacations in Florida and Arizona. Option Care supports Lydia by working with her to ensure she has access to necessary medications while she’s traveling.
“I can get out and get back a little bit of my life that I had before,” Lydia said. “It’s important to spend your energy on trying to get yourself better. Option Care home infusion helps me do that.”

Apoyo nutricional
PHOENIX, March 21, 2019 — Clinical interventions provided by a nutrition support team can prevent hospital readmission in patients with short bowel syndrome (SBS) receiving home parenteral nutrition (PN), saving millions in costs annually, suggests a study[*]Englert M, Stodola K. Proactive Interventions by Nutrition Support Clinicians in Patients with Short Bowel Syndrome (SBS) on Home Parenteral Nutrition (HPN) Results in Decreased Hospitalizations and Improved Financial Outcomes. Abstract presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference; March 23-26, 2019, Phoenix. by Option Care Enterprises, Inc. ( “Option Care”), the nation’s leading provider of home and alternate site infusion therapy services. The research is being presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference and was chosen as an Abstract of Distinction.
Among SBS patients receiving home PN provided intravenously (IV), dehydration is a common cause of hospital readmission, with an average three-day length of stay. In the study, the nutrition support team — including a dietitian, nurse and pharmacist — made recommendations (interventions) to adjust the home PN volume based on the weekly monitoring of patients’ hydration status through reviewing laboratory values and conducting nutrition assessments.
“Home nutrition patients on PN with SBS need to be observed closely the first month to prevent dehydration and making appropriate adjustments to the home PN volume is essential,” said Mary Englert, MS, RD, CSO, LDN, CNSC, Area Lead, Nutrition Support Dietitian at Option Care and lead author of the study. “Every intervention decreases the likelihood of the patient being readmitted to the hospital and this study highlights the value of a nutrition team in providing clinical monitoring and nutrition support, which leads to improved patient care and significant cost savings.”
The study included 116 patients with SBS who received home PN after being discharged from the hospital. The Registered Dietitian-led nutrition support team provided ongoing evaluation by reviewing labs weekly and conducting a thorough nutrition assessment, recommending adjustments to the volume of PN when indicated for a total of 63 proactive interventions during the four-week review period. The most common reasons for home PN volume adjustments were: to meet the patient’s estimated fluid needs (56 percent); lab values reflecting dehydration (22 percent) and increased gastrointestinal output (22 percent).
Only 14 of the study patients were readmitted to the hospital within two weeks of discharge, none resulting from dehydration. Readmissions were due to: abscess/infection not related to PN (35.7 percent); line infection/replacement (21.4 percent); bowel obstruction (14.3 percent) and nausea/vomiting, feeding tube replacement, chest pain and unknown (7.1 percent each).
The researchers determined the interventions correlated to 189 hospital days prevented and $378,000 in costs saved in one month. Projected over one year that equates to 2,268 hospital days prevented and over $4.5 million in savings.
Also presented at ASPEN:
In another Option Care study[*]Hughey M, Corey B. Early Clinical Intervention Increases Compliance and Decreases Unnecessary Discontinuation in SBS Patients treated with Teduglutide. Abstract presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference; March 23-26, 2019, Phoenix. presented at ASPEN, 162 SBS patients were proactively screened for appropriate dosing before receiving teduglutide, which helps increase fluid and nutrient absorption resulting in decreased dependence on Parenteral Support. The clinical intervention resulted in recommended reductions to the prescribed dose in 64 of the patients (40 percent), half of which were based on impaired kidney function. Ensuring patients receive the appropriate dose reduces potential therapy complications including fluid overload, worsening kidney function and premature therapy discontinuation.
Acerca de Option Care
Option Care Enterprises, Inc. (Option Care) is the nation’s leading and most trusted provider of home and alternate site infusion therapy services. Holding accreditations from industry quality organizations ACHC, PCAB, ASHP and URAC,[*]Accreditation Commission for Health Care (ACHC), Pharmacy Compounding Accreditation Board (PCAB), American Society of Health-System Pharmacists (ASHP) and URAC the company draws on nearly 40 years of clinical care experience to offer patient-centered therapy management. Option Care’s signature infusion services include the clinical management of infusion medicines, nursing support and care coordination. Option Care’s multidisciplinary team of more than 1,800 clinicians — including pharmacists, nurses and dietitians — are able to provide infusion service coverage for nearly all patients across the United States needing treatment for complex and chronic conditions. Learn more at www.OptionCare.com.

Apoyo nutricional
Estudio de Option Care revela que muchas veces se receta a los pacientes nutrición en el hogar que no satisface sus necesidades
Una investigación presentada en la Semana de la Nutrición Clínica sugiere que una receta incorrecta puede provocar sobrealimentación, subalimentación, riesgos a la salud y mayores costos
 ORLANDO, Fla., Feb. 9, 2017 — Nutrition support orders upon discharge from the hospital often don’t meet the needs of patients, according to Option Care data being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. If nutrition support orders are not corrected, patients may be overfed or underfed, both of which put them at health risk and in the case of overfeeding, adds unnecessary costs.
ORLANDO, Fla., Feb. 9, 2017 — Nutrition support orders upon discharge from the hospital often don’t meet the needs of patients, according to Option Care data being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. If nutrition support orders are not corrected, patients may be overfed or underfed, both of which put them at health risk and in the case of overfeeding, adds unnecessary costs.
Los investigadores de Option Care determinaron que las prescripciones de egreso para nutrición parenteral en el hogar (intravenosa) no satisfacían las necesidades de los pacientes casi una de cada cuatro veces. Si bien fue mayor la probabilidad de satisfacer las necesidades nutricionales para la nutrición enteral en el hogar (por sonda de alimentación), el 38 por ciento de las prescripciones no cumplía las necesidades de líquidos (hidratación). Los nutricionistas certificados de Option Care revisaron todas las prescripciones, realizaron evaluaciones nutricionales cuando los pacientes recibieron el alta para ser atendidos en el hogar y cambiaron la prescripción de nutrición en la forma recomendada si se justificaba, en función de los valores de laboratorio, el nivel de actividad y el estado de salud general del paciente.
“Nutrition support is complex and quality patient care provided in the home setting requires close collaboration between referring clinicians and a qualified home nutrition support team that has nutrition support expertise, including a registered dietitian, pharmacist and nurse,” said Noreen Luszcz, RD, MBA, CNSC, lead author of the study and nutrition program director for Option Care. “When a patient leaves the hospital, it is vital that the home infusion dietitian complete a nutrition assessment to ensure the order follows A.S.P.E.N. guidelines and the patient’s current needs are being met.”
La sobrealimentación puede causar problemas metabólicos y un exceso de aumento de peso, además de incrementar los costos al proporcionar más nutrición de la necesaria. Los pacientes subalimentados pueden no aumentar de peso adecuadamente o no recuperarse con la rapidez que deberían.
Nombrado póster distinguido en la CNW de A.S.P.E.N. por excelencia e innovación, la investigación comprendió el análisis de las prescripciones nutricionales de 187 pacientes de nutrición parenteral en el hogar y 349 pacientes de nutrición enteral en el hogar
que fueron dados de alta en hospitales que no contaban con equipos dedicados de apoyo nutricional para aconsejar en la prescripción.
Para los 187 pacientes de nutrición parenteral en el hogar de Option Care, los investigadores determinaron que las prescripciones originales no satisfacían las necesidades de los pacientes, en promedio, un 23 % de las veces. Las conclusiones fueron las siguientes:
- 41 (22 por ciento) no cumplieron las necesidades de líquido;
- 48 (26 por ciento) no cumplieron las necesidades de aminoácidos (proteínas);
- 39 (21 por ciento) no cumplieron las necesidades de dextrosa (carbohidratos);
- 34 (18 por ciento) no cumplieron las necesidades de lípidos (grasas) y
- 51 (27 por ciento) no cumplieron las necesidades calóricas totales.
Además, se recetó erróneamente nutrición parenteral en el hogar a 24 pacientes (13 por ciento) que deberían haber recibido nutrición mediante otras vías menos costosas, como la nutrición enteral en el hogar o la ingesta oral. La nutrición parenteral en el hogar debe recetarse solamente a los pacientes cuyos sistemas gastrointestinales no pueden procesar los nutrientes de forma adecuada. Los dos principales médicos prescriptores fueron especialistas en medicina interna (29 por ciento) y gastroenterólogos (19 por ciento).
En el caso de las proteínas, los pacientes recibieron inicialmente prescripciones que habrían provocado sobrealimentación el 48 por ciento de las veces y subalimentación el 52 por ciento de las veces. En las categorías restantes, fue mucho más probable que los pacientes recibieran inicialmente prescripciones que habrían provocado subalimentación. Los investigadores estiman que la cantidad promedio de exceso de proteínas recetadas tendría como consecuencia un costo de 179 837 USD adicionales por paciente que recibió terapia de nutrición parenteral en el hogar durante 90 días, la duración promedio de la terapia. Se determinó que corregir la receta de proteínas en el 12 por ciento de las prescripciones de nutrición parenteral en el hogar únicamente tendría como resultado un ahorro en costos de asistencia médica de 5,2 millones de USD.
Entre los 349 pacientes de nutrición enteral en el hogar de Option Care, los investigadores que evaluaron las prescripciones originales determinaron lo siguiente:
- 133 (38 por ciento) no incluían la prescripción de irrigación con agua (de manera que el paciente no habría recibido suficiente líquido);
- a 15 (4 por ciento) se les recetaron fórmulas que no eran las más adecuadas para su afección;
- 10 (2 por ciento) hubieran sido sobrealimentados y
- 18 (5 por ciento) hubieran sido subalimentados.
Los investigadores observan que hay varios factores que pueden llevar a que las recetas de nutrición tras el alta del hospital no satisfagan las necesidades del paciente. Muchas veces, son los médicos quienes hacen las recetas, y es posible que no cuenten con conocimientos especializados en nutrición y no tengan un equipo de apoyo nutricional cualificado, formado por un nutricionista matriculado, enfermero y farmacéutico, para guiarlos. Además, las necesidades nutricionales cambian con el tiempo. Un paciente con una lesión aguda puede necesitar más proteínas mientras se esté curando, pero dicha necesidad puede disminuir en el momento de recibir el alta para volver a casa. Si no se ajusta la receta, la persona puede recibir un nivel inadecuado de proteínas, que aumentan con el tiempo. Finalmente, se da un alto nivel de escrutinio para determinar si un paciente cumple los requisitos para el apoyo nutricional en el hogar (especialmente con Medicare), mientras que los hospitales no son sometidos al mismo nivel de evaluación.
El programa e apoyo nutricional de Option Care practica un enfoque de equipo multidisciplinario para la atención que incluye enfermeros, farmacéuticos y nutricionistas certificados en apoyo nutricional, quienes trabajan en estrecha colaboración con los médicos para brindar atención de la más alta calidad a los pacientes de nutrición parenteral y enteral en el hogar. Cada centro de gestión de la atención recibe el apoyo de un nutricionista certificado en todo el país.
A los pacientes se les receta nutrición parenteral porque no pueden satisfacer sus necesidades nutricionales oralmente debido a afecciones tales como cáncer, accidente cerebrovascular, trastornos gastrointestinales o complicaciones quirúrgicas. Ambas terapias se pueden administrar temporariamente en el hospital; sin embargo, unos 40 000 pacientes de nutrición parenteral en el hogar y 344 000 pacientes de nutrición enteral en el hogar por año reciben terapia de nutrición de forma segura y con menos costos en su hogar, lo que evita el riesgo de exposición a infecciones intrahospitalarias y permite volver al trabajo y a una vida activa. Aunque algunas personas reciben estas terapias por un período corto, muchos deben hacerlo a largo plazo y algunos durante toda la vida.
Acerca de Option Care
Option Care Enterprises, Inc. (Option Care) es uno de los proveedores de servicios de infusión en el hogar y en centros alternativos de tratamiento más grandes y más confiables del país. Como líder en la industria, la empresa se respalda en casi 40 años de experiencia en atención clínica para ofrecer gestión de la terapia basada en el paciente. Los servicios distintivos de Option Care, Home Infusion Plus, comprenden la administración clínica de los medicamentos de infusión, el apoyo de enfermeros y la coordinación de la atención. El equipo multidisciplinario de más de 1,800 profesionales clínicos de Option Care, formado por farmacéuticos, enfermeros y nutricionistas, puede proporcionar cobertura de servicios de infusión en el hogar para casi todos los pacientes en los Estados Unidos que necesiten tratamiento para afecciones complejas y crónicas. Obtenga más información en www.OptionCare.com.

Apoyo nutricional
Many Home Parenteral Nutrition Patients Denied Medicare Reimbursement a pesar de que reciben tratamiento según las pautas de A.S.P.E.N.
Un estudio de Option Care subraya la necesidad de alinear atención con cobertura
 ORLANDO, Fla., Feb. 9, 2017 — Many home parenteral nutrition (HPN) patients who struggle to gain or maintain weight due to complex medical conditions may be falling through the cracks due to an outdated Medicare qualification process, suggests Option Care research being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. The study determined that Medicare coverage often doesn’t match up with A.S.P.E.N. guideline recommendations, forcing patients to pay for some or all of their life-saving care.
ORLANDO, Fla., Feb. 9, 2017 — Many home parenteral nutrition (HPN) patients who struggle to gain or maintain weight due to complex medical conditions may be falling through the cracks due to an outdated Medicare qualification process, suggests Option Care research being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. The study determined that Medicare coverage often doesn’t match up with A.S.P.E.N. guideline recommendations, forcing patients to pay for some or all of their life-saving care.
Los investigadores hallaron que más de la mitad de los pacientes de nutrición parenteral en el hogar (intravenosa) cuya atención cumplía las pautas de A.S.P.E.N. (American Society for Parenteral and Enteral Nutrition, Asociación Estadounidense para la Nutrición Parenteral y Enteral) no reunían los requisitos para la cobertura de Medicare. Los hallazgos sugieren que Medicare utiliza criterios anticuados para sus requisitos en cuanto a nutrición parenteral en el hogar, como herramientas de diagnóstico de desnutrición que no reflejan la atención recomendada actualmente.
“HPN is an expensive therapy and understandably Medicare wants to ensure that patients require that level of nutrition,” said Natalie S. Tu, RD, lead author of the study and clinical nutrition support dietitian for Option Care. “However, many malnourished patients have a clear need for HPN but don’t qualify for Medicare coverage. Care team members — including doctors and dietitians — need to diligently document the patient’s need in an attempt to secure Medicare coverage.”
In some cases, appeals providing additional documentation of need may be successful in securing coverage for patients initially denied by Medicare. Medicare patients who don’t qualify for coverage pay out of pocket costs which can be up to $250 a day and are prohibitive for many people. The average length of therapy for Option Care HPN patients is three months.[*] Option Care data on file.Patients who have supplemental insurance may be partially covered, but will be required to pay a daily deductible, which also adds up.
Actualmente, cerca del 20 por ciento de los pacientes de nutrición parenteral de Option Care tienen Medicare. "Este porcentaje seguirá creciendo a medida que la población envejezca, lo que subraya la necesidad de alinear mejor la cobertura de Medicare con las pautas de A.S.P.E.N.", comentó Tu.
El estudio de Option Care fue nombrado como resumen de distinción para la excelencia y la innovación de la CNW de A.S.P.E.N. Los investigadores analizaron a 142 pacientes que recibían nutrición parenteral, y hallaron que 49 (el 35 por ciento) reunían los requisitos de selección de Medicare para nutrición parenteral y 56 (el 39 por ciento) no, mientras que 37 (el 26 por ciento) no avanzaron con los procedimientos porque el proceso de selección fue interrumpido o estaba incompleto. De los 56 pacientes que no reunían los requisitos para Medicare, 31 (el 55 por ciento) cumplía con las pautas que recomienda A.S.P.E.N.
A los pacientes se les receta nutrición parenteral porque no pueden satisfacer sus necesidades nutricionales oralmente o mediante una sonda de alimentación (nutrición enteral) debido a afecciones tales como cáncer, accidente cerebrovascular, trastornos gastrointestinales o complicaciones quirúrgicas. Si bien la nutrición parenteral se puede administrar en el hospital, unos 40 000 pacientes por año reciben terapia de nutrición de forma segura y con menos costos en su hogar, lo que evita el riesgo de exposición a infecciones intrahospitalarias y permite volver al trabajo y a una vida activa.
El programa e apoyo nutricional de Option Care practica un enfoque de equipo multidisciplinario para la atención que incluye enfermeros, farmacéuticos y nutricionistas certificados en apoyo nutricional, quienes trabajan en estrecha colaboración con los médicos para brindar atención de la más alta calidad a los pacientes de nutrición en el hogar. Cada centro de gestión de la atención recibe el apoyo de un nutricionista matriculado en todo el país.
Acerca de Option Care
Option Care Enterprises, Inc. (Option Care) is one of the nation’s largest and most trusted providers of home and alternate treatment site infusion services. An industry leader, the company draws on nearly 40 years of clinical care experience to offer patient-centered therapy management. Option Care’s signature Home Infusion Plus services include the clinical management of infusion medicines, nursing support and care coordination. Option Care’s multidisciplinary team of more than 1,800 clinicians — including pharmacists, nurses and dietitians — are able to provide home infusion service coverage for nearly all patients across the United States needing treatment for complex and chronic conditions. Learn more at www.OptionCare.com.
# # #

Apoyo nutricional
BANNOCKBURN, Ill., June 2, 2016 — Option Care Enterprises, Inc., a leading national provider of home and alternate treatment site infusion therapy, has been selected by the Centers for Medicare & Medicaid Services (CMS) to continue to provide home enteral (tube feeding) nutrition services to Medicare patients across the country.
A través de un proceso competitivo de licitación, los CMS otorgan contratos a proveedores de Medicare que cumplen estándares específicos financieros y de calidad. Option Care proporciona nutrición enteral en el hogar a pacientes de Medicare desde el lanzamiento del programa competitivo de licitación de los CMS en 2011.
"Ser constantemente seleccionados por los CMS prueba que Option Care es un socio preferido, porque nuestra trayectoria proporcionando atención de calidad garantiza resultados exitosos", comentó John Rademacher, Director de Operaciones de Option Care. "Nuestras altas tasas de satisfacción del paciente y de seguridad demuestran que ponemos a los pacientes en el centro de nuestro enfoque personalizado y humano de la atención". "
El programa competitivo de licitación de los CMS se lanzó en las primeras nueve áreas metropolitanas en 2011, y, a partir de 1.º de julio, abarcará 117 áreas. Forma parte de un programa que exige el Congreso mediante la Ley de Modernización y Mejora de Medicamentos de Venta con Receta de Medicare (Medicare Prescription Drug, Improvement and Modernization Act) de 2003. Este programa competitivo de licitación para determinados equipos médicos duraderos, prótesis, equipos ortopédicos e insumos tiene como objetivo reducir los gastos a cargo del paciente y garantizar que reciba servicios de calidad. También busca ahorrar costos a Medicare.
El equipo de apoyo nutricional de Option Care está formado por más de 1800 profesionales clínicos y 100 nutricionistas en todo el país, y su equipo de liderazgo tiene, en forma conjunta, más de 125 años de experiencia proporcionando terapia de nutrición en el hogar. Mediante el programa de alimentación por sonda en el hogar de intervención temprana, Option Care cubre las posibles lagunas en la atención al eliminar los obstáculos financieros, realizar evaluaciones nutricionales individualizadas y brindar educación al paciente aun antes de que empiece la terapia.
Option Care brinda apoyo nutricional enteral en el hogar, además de apoyo nutricional parenteral (intravenoso) en el hogar, para pacientes con numerosas afecciones agudas y crónicas que afectan negativamente su salud nutricional. Entre estas afecciones podemos nombrar el accidente cerebrovascular, el cáncer y las enfermedades gastrointestinales.
En terapia nutricional en el hogar, se ha demostrado que los servicios y estándares altos de Option Care evitan la hospitalización y reducen los costos. Un estudio de Option Care realizado en 2016 determinó que la monitorización minuciosa y la gestión proactiva de 126 pacientes de nutrición enteral en el hogar y 124 pacientes de nutrición parenteral en el hogar llevaron a realizar intervenciones que permitieron evitar 957 días de hospital, lo que significa un ahorro de más de 1,9 millones de USD. Entre las intervenciones se pueden mencionar el manejo de la hiperglucemia o del desequilibrio hidroelectrolítico, la prevención de la deshidratación y la reducción o eliminación de la diarrea.
Option Care se dedica a prestar servicios de atención de la salud en el hogar de la más alta calidad para pacientes pediátricos y adultos que necesitan terapias de infusión con el fin de tratar una amplia gama de afecciones complejas y agudas. Además de brindar servicios de nutrición en el hogar, Option Care proporciona infusión en el hogar para tratar diversas afecciones, desde enfermedades infecciosas, cáncer y deficiencias inmunitarias primarias hasta trastornos autoinmunitarios e insuficiencia orgánica terminal.
Acerca de Option Care
Option Care Enterprises, Inc. (Option Care) is one of the nation’s largest and most trusted providers of home and alternate treatment site infusion services. An industry leader, the company draws on nearly 40 years of clinical care experience to offer patient-centered therapy management. Option Care’s signature Home Infusion Plus services include the clinical management of infusion medicines, nursing support and care coordination. Option Care’s multidisciplinary team of more than 1,800 clinicians — including pharmacists, nurses and dietitians — are able to provide home infusion service coverage for nearly all patients across the United States needing treatment for complex and chronic conditions. Learn more at www.OptionCare.com.
# # #